Learning more about Plantar Fasciitis
On face value, your feet touch the ground whenever you are standing, walking or running. Our feet are extensions of our legs, which help move you. Our feet are the foundation of our bodies, which means keeping your feet healthy, keeps you healthy.
In our lifetime, the average person walks approximately 160,000 kilometres. But all too often, we do not place the same emphasis on looking after our feet as we do on other parts of our body. “Keeping your feet healthy should be part of your daily routine, just because they are furthest away from your eyes should not mean you should neglect them!”1
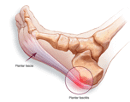
Overuse injuries of the foot may lead to plantar fasciitis, which is one of the most common causes of heel pain. Plantar fasciitis involves inflammation of the plantar fascia
Fasciitis is the most common injury of the plantar fascia and is estimated to induce more than 1 million patients to seek treatment every year.5 The plantar fascia is a thick, ligamentous structure that runs from the bottom of the heel, across the foot to the toes. The fascia is the largest ligament in the human body, designed in the shape of a bowstring which supports the footbridge, absorbing the shock when walking.2,3 The fascia consists of 3 bundles, central, lateral and medial. The central component is proximally thick and distally thin and is the thickest of the three. These large fibrous bundles are embedded within a matrix of loose connective tissue containing type III collagen and a few elastic fibres. 4
Plantar fasciitis can develop without obvious causes; however, some factors may increase your risk of developing plantar fasciitis.
Risk factors include
- Most common between the ages of 40-60 years.2
- Certain types of exercise. Plantar fasciitis is common in runners, however, activities resulting in stress on the heel, for example, ballet dancing may contribute to the onset of plantar fasciitis.2
- Foot mechanics. People with foot deformities (flat feet, high arch, abnormal walking pattern) are also at risk of developing plantar fasciitis. Some underlying medical conditions such as spondyloarthropathies and rheumatoid arthritis are also associated with plantar fasciitis.2,4
- Extra weight puts extra stress on the plantar fascia.
- People who spend most of their work hours walking or standing on hard surfaces for example factory worker’s or teachers are more at risk of developing plantar fasciitis.2
- Bony growths or spurring at the bottom part of the heel (calcaneal enthesophytes), is likely a possible cause.4
Clinical diagnosis
General diagnosis of plantar fasciitis relies on the clinical history and physical examination. The most common complaint is pain on the bottom surface of the heel during weight-bearing. Pain is usually worse after resting periods, therefore patients experience stiffness and pain in the morning, or at the beginning of an activity, but eases with walking. The passive pulling back of the toes (dorsiflexion) exacerbates the pain.4,6
Successful outcome rests on the adequate diagnosis and focused treatment for the best possible recovery:

Plain radiograph
General x-rays are non-specific; however, calcaneal spurring is well visualised.6

Ultrasound
Ultrasound is the imaging modality of choice, which shows the increased thickness of the plantar fascia (more than 4.5 mm) with disturbance of the normal echo pattern. Intrasubstance tendon tears can also be well visualized. 6
Magnetic Resonance Imaging (MRI)
Affected areas appear swollen with plantar fascia thickening, usually indicating the involvement of the proximal portion of the plantar fascia. Underlying swollen areas or inflammatory changes in the fat pad of the foot as well as bone marrow oedema is well visualized. 6
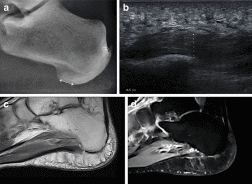
Imaging modalities. (a) Plain radiograph, (b) Thickening of the plantar fascia on ultrasound image, (c,d) MRI images to confirm plantar fasciitis at the origin4
Treatment:
- RICE method:
- REST for a few days
- ICE the bottom part of the foot for 20 minutes at the time
- COMPRESS the area to reduce swelling
- ELEVATE the foot.7
- Anti-inflammatory medication/infiltration
Non-steroidal anti-inflammatory drugs 9(NSAID’S) may reduce pain and inflammation.7 Local injection of steroids +/- local anaesthetic may be useful to manage symptoms, shown to be effective in short-term pain relief with long-term reduced thickness of the plantar fascia. Corticosteroid injection has been shown to be more effective when done under ultrasound guidance. Ultrasound-guided steroid injection has been shown to be effective in short-term (four-week) pain relief with reduced thickness of the plantar fascia at three months.2,6
- Shoe inserts
Additional support of the foot arch is provided by shoe inserts, especially effective in people who spend most of the day on the feet. Consult with a podiatrist or orthopedic surgeon for more information.6
- Massage
Massage of the foot arch and surrounding soft tissue may help to release tension.
- Plantar fascia stretches
- Stretching the calf muscles release muscle tightness in the feet and calves and may relieve pain.2,6
- Rolling stretches –rolling back and forth a golf/tennis ball or specialized foam roller to release tension under the foot. 2,6
- Stretching of the plantar fascia: Cross the injured foot over the opposite leg and pull the toes back to release tension in the arch of the foot. 2,6
- Foot flexes: Sit flat on the floor with the leg stretched out in front of you. Rap an elastic band around the forefoot and gently pull the toes toward the body.
- Towel curls: Sitting on a chair, grasp a hand towel with your toes and curl the towel towards you. 2,6
- Marble pickups: Pic marbles up with your to, one at the time by curling your toes and place the marbles into bowl. 2,6
Prognosis and complications
Ongoing and chronic plantar fasciitis may result in chronic heel pain and plantar fascia tears. Long-standing changes in the way you walk might lead to other problems involving the foot, head, knee and back.2
If you suspect plantar fasciitis or would like to know more about diagnosis and imaging of plantar fasciitis, reach out to Keystone Radiology at 087 055 0587 or info@ks-med.co.za
Make a booking
REFERENCES
- The Pharmaceutical Journal [Internet]. A strong base: the importance of foot health. 2017. [cited 30 September 2020]. Available from: https://www.pharmaceutical-journal.com/publications/supplements/focus-foot-health/a-strong-base-the-importance-of-foot-health/20203182.article?firstPass=false
- The Mayo Clinic [Internet]. Exercises to help prevent plantar fasciitis. [cited 30 September 2020]. Available from: https://www.mayoclinic.org/diseases-conditions/plantar-fasciitis/symptoms-causes/syc-20354846
- MedicineNet [Internet]. Plantar Fasciitis. [cited 30 September 2020]. Available from: https://www.medicinenet.com/plantar_fasciitis/article.htm
- Draghi F, Gitto S, Bortolotto C, Draghi AG, Belometti GO. Imaging of plantar fascia disorders: findings on plain radiography, ultrasound and magnetic resonance imaging. Imaging Insights. 2017; Feb; 8(1): 69–78.
- Riddle DL, Schappert SM. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int. 2004;25(5):303–310.
- Radiopaedia [Internet]. Plantar Fasciitis. [cited 30 September 2020]. Available from: https://radiopaedia.org/articles/plantar-fasciitis
- Medical News Today [Internet]. Best exercises and remedies for plantar fasciitis. [cited 30 September 2020]. Available from: http://medicalnewstoday.com/articles/324353.