The Interplay between the Endocrine and Skeletal System
The thyroid
A butterfly-shaped, endocrine gland located in the front of the neck just below the Adam’s apple. It collects iodine from the bloodstream and further produce hormones that are important for growth and energy metabolism of the body.8
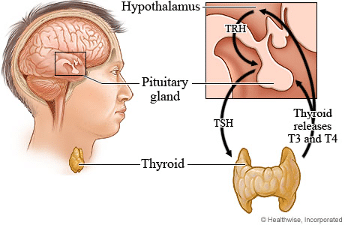
After collecting iodine from nutrition, the iodine fuels the thyroid to produce thyroxine (T4) and triiodothyronine (T3). Thyroid hormone metabolism and production is a complex symphony of T3/T4 in the body, thyrotropin-releasing hormone (TRH) from the Hypothalamus and thyroid stimulating hormone (TSH) from the pituitary gland. TSH stimulates the thyroid to collect iodine and produce T3/T4. The release of TRH is stopped when T3/T4 levels are normal. 8
Thyroid malfunctioning arises when the thyroid overproduces or underproduces hormones or when structural changes occur, such as the development of a lump (known as a nodule) or thyroid enlargement (known as a goiter).
Thyroid hormone level Classifications:
1. Euthyroidism
Refers to a normal functioning thyroid with normal TSH and T3/T4 hormone levels in the blood.4,6
2. Hypothyroidism
An underactive thyroid cannot meet the body’s needs and as a result, slows down many of the metabolic processes of the body. The inability of the thyroid to produce the necessary hormones for normal functioning also has a direct influence on skin and bone health.
Symptoms include:
- A Goiter (enlarged thyroid)
- Feel cold
- Depressed
- Fatigue
- Weight gain
- Hair loss/dry & brittle
- Dry skin and Brittle nails
- Muscle cramps
- Constipation
- Irregular menstruation
- A slow heartrate and metabolism.4,6
3. Hyperthyroidism
It is the overactive and excessive production of thyroid hormones. The thyroid may go in over-drive and produce excessive hormones, resulting in speeding up of the body’s normal processes.
This may present as:
- Sweating
- Increased bowel movements/diarrhoea
- Increased heart rate
- Unexplained weight loss
- Anxiety
- Headache
- Tremors/Shaking
- Itchy red skin
- Heat intolerance4,
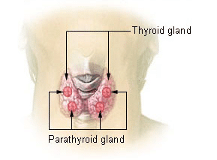
The parathyroid glands
Four tiny glands, located in the neck, adjacent to the thyroid gland. They are responsible for regulating Calcium levels of the body and therefore have a direct effect on bone health.
Muscles and energy metabolism as well as bone mass density are under direct influence of the thyroid and parathyroid glands.8

The skeletal system
Bone acts as a reservoir for bone cells. Bone cells are formed by osteoblasts which are building cells. It can also be broken down by osteoclasts that act as destroying cells. The process of building or breaking of bone cells is ongoing and normally takes 200 days to complete one cycle. A well-balanced bone turnover is vital for keeping a healthy bone metabolism.1,6
Bone density is classified according to three states:
- Normal
- Osteopaenic: Osteopenia refers to a loss of bone. This may progress to osteoporosis.
- Osteoporosis: Osteoporosis means porous bone. It describes the state of fragile bones due to increased bone loss, decreased bone production or both and is associated with an increased risk of bone fractures.2
Candidates that are generally at risk of low bone density include:
- Caucasian or Asian females
- Premature menopause
- Vitamin D deficiency
- Lack of exercise
- Steroid intake
- Cigarette smoking, excessive alcohol consumption and a low body weight may also increase the risk.3,6
At Keystone Radiology, we offer the following screening and diagnostic services
1. Ultrasound

- This non-invasive, radiation-free modality provides information on the size and appearance of the thyroid gland. Certain characteristics identifiable on ultrasound are pathognomonic for certain thyroid and parathyroid lesions.
- Autoimmune diseases and malignancies can be identified by a change in structural appearance. The parathyroid glands can also be visualized using this modality. Surrounding soft tissue and masses or abnormalities can also be visualized.
- Inflammation of the thyroid gland known as thyroiditis and autoimmune diseases can be assessed. An overall appearance of irregular thyroid tissue or multiple small nodules and an increase in blood supply may indicate an autoimmune disease.11
- Ultrasound screening can be followed by a thyroid function blood test or biopsy.
2. DEXA SCAN
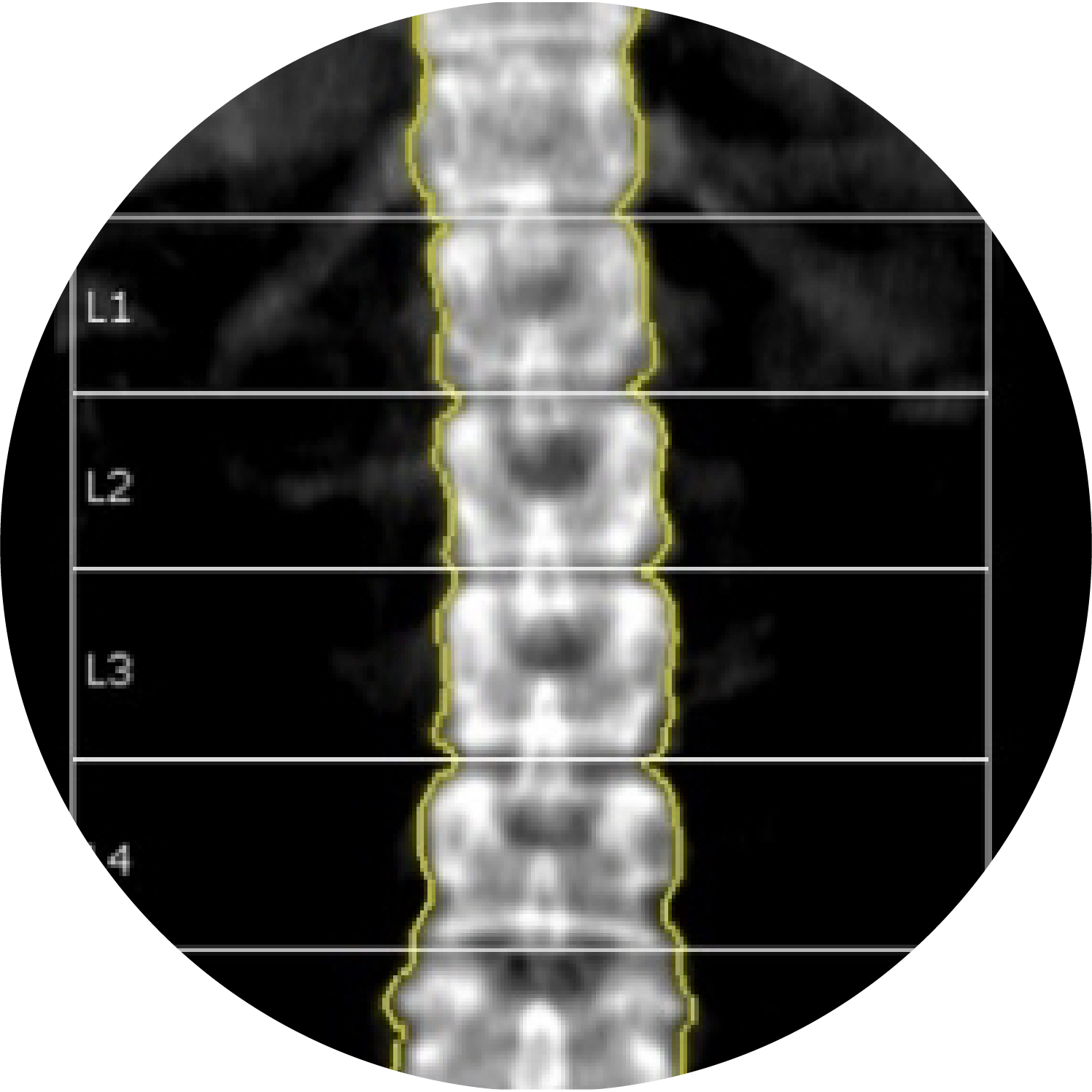
Bone strength and density can be measured by means of a DEXA scan (dual-energy x-ray absorptiometry).2
Our state-of-the-art Body composition Analysis Scanner allows the opportunity to assess
- Bone Density (DEXA)
- Fat composition
- Metabolic rates
- Corescan
- Android and Gynoid Ratio
A DEXA scan uses a very low dose of X-ray to measure the density of the skeletal system and to determine your risk for developing osteoporosis. The scan data can also be used for assessing the total composition of the body, including the fat and muscle percentages. DEXA is considered the gold standard in measuring body composition.
For more information and to book your appointment at Keystone Radiology, contact us on 087 055 0587 or info@ks-med.co.za
Make a booking
Bibliography:
- Nowak, T., 2004. Pathophysiology: Concepts and Applications For Health Care Professionals. 3rd ed. United States: Mcgraw-Hill.
- Harris S, Bollerslev J, Martinez R. Medicine Induced Bone Loss | Endocrine Society [Internet]. Hormone.org. 2020 [cited 18 March 2020]. Available from: https://www.hormone.org/diseases-and-conditions/osteoporosis/medicine-induced-bone-loss
- Senderovich H, Kosmopoulos A. An Insight into the Effect of Exercises on the Prevention of Osteoporosis and Associated Fractures in High-risk Individuals [Internet]. Rambam Maimonides Medical Journal. 2018 [cited 18 March 2020]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5796736/
- About Your Thyroid [Internet]. Empower your Health. 2020 [cited 19 March 2020]. Available from: https://www.empoweryourhealth.org/Overactive-Thyroid
- Moore, K., Agur, A. and Dalley, A., 2006. Clinically Oriented Anatomy. 5th ed. Lippincott Williams & Wilkins.
- Thyroid disease and osteoporosis: Consumer factsheet [Internet]. Osteoporosis Australia. 2020 [cited 19 March 2020]. Available from: https://www.osteoporosis.org.au/sites/default/files/files/Thyroid%20factsheet(1).pdf
- Daly R, Dalla Via J, Duckham R, Fraser S, Wullf Helge E. Exercise for the prevention of osteoporosis in postmenopausal women: an evidence-based guide to the optimal prescription [Internet]. National Center for Biotechnology Information. 2018 [cited 21 March 2020]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6429007/
- Medical Media. Thyroid gland – What’s the function of the thyroid? [Internet]. 2020 [cited 22 March 2020]. Available from: https://www.youtube.com/watch?v=xKQa-MbZUPY
- Health Wise. Thyroid Hormone Production – Metro Health Hospital Metro Health [Internet]. 2019 [cited 22 March 2020]. Available from: http://google.com/imgres?imgurl=https%3A%2F%2Fcontent.healthwise.net%2Fresources%2F12.4%2Fen-us%2Fmedia%2Fmedical%2Fhw%2Fh9991509_001.jpg&imgrefurl=https%3A%2F%2Fmetrohealth.net%2Fhealthwise%2Fthyroid-hormone-production%2F&tbnid=oY4x4QDAvbQsGM&vet=12ahUKEwikgoqVvK7oAhVQ4oUKH
- WebMD. Hypothyroidism (Underactive Thyroid) [Internet].2019 [cited 22 March 2020]. Available from: https://www.webmd.com/women/hypothyroidism-underactive-thyroid-symptoms-causes-treatments#1
- F. Gaillard, Z. Sabahi. Thyroid gland. [Internet]. Radiopaedia. 2020 [cited 20 March 2020]. Available from: https://radiopaedia.org/articles/thyroid-gland